

875 mg PO q12hr or 500 mg PO q8hr for 10-14 days
H pylori infection and active or 1-year history of duodenal ulcer
Postexposure inhalational prophylaxis
500 mg PO q8hr
Prophylaxis
2 g PO 30-60 min before procedure
Erythema migrans and other symptoms of early dissemination
500 mg PO q8hr (depending on size of patient) for 3-4week
50 mg/kg/day q8hr in divided doses; maximum 500 mg/dose
First trimester: 500 mg PO q8hr for 7 days
First trimester: Test to document chlamydial eradication and retest for infection 3 months after treatment
Second or third trimester: Test to document chlamydial eradication
AHA guidelines recommend prophylaxis only in high-risk patients undergoing invasive procedures who have a history of cardiac conditions that predispose them to a risk of infection
Anaphylaxis
Anemia
AST/ALT elevation
Mucocutaneous candidiasis
Diarrhea
Headache
Nausea
Vomiting
Rash
Pseudomembranous colitis
Serum sickness-like reactions
Mucocutaneous candidiasis
Gastrointestinal (eg, black hairy tongue and hemorrhagic/pseudomembranous colitis, which may occur during or after treatment)
Hypersensitivity reactions, anaphylactic/anaphylactoid reactions (including shock), angioedema, serum sickness-like reactions (urticaria or skin rash accompanied by arthritis, arthralgia, myalgia, and frequently fever), hypersensitivity vasculitis, erythematous maculopapular rashes, erythema multiforme, Stevens-Johnson syndrome, exfoliative dermatitis, toxic epidermal necrolysis, acute generalized exanthematous pustulosis, hypersensitivity vasculitis, urticaria, pruritis, DRESS
Moderate increase in AST and/or ALT; hepatic dysfunction (eg, cholestatic jaundice, hepatic cholestasis, and acute cytolytic hepatitis have been reported)
Renal (eg, crystalluria)
Anemia (eg, hemolytic anemia, thrombocytopenia, thrombocytopenic purpura, eosinophilia, leukopenia, agranulocytosis)
CNS reactions (eg, reversible hyperactivity, agitation, anxiety, insomnia, confusion, convulsions, behavioral changes, dizziness), aseptic meningitis
Tooth discoloration (brown, yellow, or gray staining); may be reduced or eliminated with brushing or dental cleaning
Documented hypersensitivity to penicillins, cephalosporins, imipenem
Anaphylaxis has been reported rarely but is more likely to occur following parenteral therapy with penicillins
Clostridium difficile-associated diarrhea (CDAD) has been reported with use of nearly all antibacterial agents; severity may range from mild diarrhea to fatal colitis; CDAD may occur over 2 months after discontinuation of therapy; if CDAD is suspected or confirmed, discontinue immediately and begin appropriate fluid and electrolyte management, protein supplementation, antibiotic treatment of C difficile, and surgical evaluation
Do not administer in patients with infectious mononucleosis because of risk of development of erythematous skin rash
Do not administer to patients in the absence of a proven or suspected bacterial infection because of risk of development of drug-resistant bacteria
Superinfections with bacterial or fungal pathogens may occur during therapy; if suspected, discontinue immediately and begin appropriate treatment
Chewable tablets contain aspartame, which contains phenylalanine
Use caution in patients with allergy to cephalosporins, carbapenems
Endocarditis prophylaxis: use for only high-risk patients, as per recent AHA guidelines
High doses may cause false urine glucose test by some methods
May cause severe cutaneous adverse reactions (SCAR), such as Stevens-Johnson syndrome (SJS), toxic epidermal necrolysis (TEN), drug reaction with eosinophilia and systemic symptoms (DRESS), and acute generalized exanthematous pustulosis (AGEP); if patients develop a skin rash they should be monitored closely and therapy discontinued if lesions progress
Available data from published epidemiologic studies and pharmacovigilance case reports over several decades with amoxicillin use have not established drug-associated risks of major birth defects, miscarriage, or adverse maternal or fetal outcomes
Data from a published clinical lactation study reports that amoxicillin is present in human milk; published adverse effects with amoxicillin exposure in breastfed infant include diarrhea
There are no data on effects of amoxicillin on milk production; the developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for therapy and any potential adverse effects on breast-fed child from drug or from underlying maternal condition
A: Generally acceptable. Controlled studies in pregnant women show no evidence of fetal risk.
B: May be acceptable. Either animal studies show no risk but human studies not available or animal studies showed minor risks and human studies done and showed no risk.C: Use with caution if benefits outweigh risks. Animal studies show risk and human studies not available or neither animal nor human studies done.
D: Use in LIFE-THREATENING emergencies when no safer drug available. Positive evidence of human fetal risk.
X: Do not use in pregnancy. Risks involved outweigh potential benefits. Safer alternatives exist.
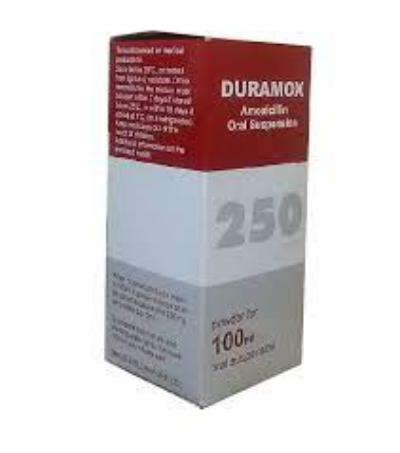
Tap bottle until all powder flows freely
Add ~1/3 of the total amount of water for reconstitution and shake vigorously to wet powder; add remaining water and again shake vigorously
May also add the required amount of suspension to formula, milk, fruit juice, water, ginger ale, or cold drinks; these preparations must be used immediately
Tablets: Take without regard to meals
Suspension: Shake well before use; may be mixed with formula, milk, fruit juice, water, ginger ale, or cold drinks; administer dose immediately after mixing
Tablets: Store at 20-25°C (68-77°F)
Prepared oral suspension: Refrigeration preferred; once reconstituted, discard 14 d